- All Drug Categories
- Home
- Anti-cancer Drugs
- Healthcare Products
- Medical Information
- Statement
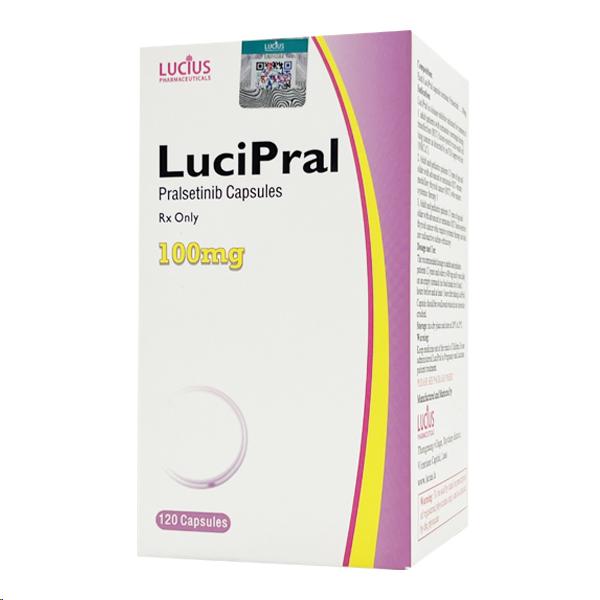
All Names: Pralsetinib、Gavreto、普吉华、普拉替尼
Indications:Treat patients with RET gene fusion-positive non-small cell lung cancer (NSCLC), medullary thyroid cancer (MTC), and other solid tumors carrying RET gene mutations
Manufacturer:LUCIUS PHARMACEUTICAL (LAOS) CO., LTD
Customs Clearance Procedure:If the customs requires the package for customs clearance, please pay the customs clearance fee according to the content of EMS SMS and customs regulations.
Pralsetinib is an oral, highly selective, and potent RET inhibitor.
1. Indications and efficacy
Pranlukast is a selective RET kinase inhibitor, suitable for the following conditions:
RET fusion-positive non-small cell lung cancer (NSCLC): Treatment for adult patients with metastatic RET fusion-positive NSCLC identified through FDA-approved testing
RET fusion-positive thyroid cancer: treatment for patients aged 12 and above with advanced or metastatic RET fusion-positive thyroid cancer who require systemic treatment and are refractory to radioactive iodine (if radioactive iodine is applicable)
This drug blocks the tumor growth signaling pathway by inhibiting RET fusion proteins and activating mutations. The indication for thyroid cancer was granted accelerated approval based on overall response rate and duration of response, and subsequent confirmatory trials are needed to confirm the clinical benefit.
II. Usage and Dosage Specification
Standard dose: 400mg orally once daily for adults and adolescents aged ≥12 years, taken on an empty stomach (fasting from 2 hours before to 1 hour after meals)
Dose adjustment: Gradually reduce the dosage to 300mg, 200mg, or 100mg once daily based on the severity of adverse reactions
Handling of missed doses: If a dose is missed on the same day, it can be taken as soon as possible, and the normal medication schedule can be resumed the next day; no need to take a missed dose after vomiting
Surgical management: Discontinue medication for at least 5 days before elective surgery, and resume medication after at least 2 weeks post-major surgery and once the wound has healed
III. Side effects and precautions
Common adverse reactions (≥25%):
Musculoskeletal pain, constipation, hypertension, diarrhea, fatigue, edema, fever, and cough
Grade 3-4 laboratory abnormalities include lymphopenia, neutropenia, decreased hemoglobin, decreased phosphate, etc
Serious risk warning:
Interstitial lung disease/pneumonia: Incidence rate is 12%, with 3.3% being grade 3-4. In case of respiratory symptoms, discontinue the medication immediately and conduct an evaluation
Hypertension: Incidence rate of 35%, with 18% being Grade 3. Blood pressure needs to be controlled before medication, and regular monitoring during treatment
Hepatotoxicity: AST increased by 49% (grade 3-4: 7%), ALT increased by 37% (grade 3-4: 4.8%). Regular monitoring of liver function is required
Bleeding events: The incidence of grade 3 or above is 4.1%, and severe bleeding requires permanent discontinuation of medication
Wound healing disorders: medication needs to be temporarily suspended before and after surgery
Embryotoxicity: Pregnant women are prohibited from using this product. Patients of childbearing age need to take effective non-hormonal contraceptive measures
IV. Medication for special populations
Children: Applicable to thyroid cancer patients aged ≥12 years, with monitoring of growth plate development required
Liver injury: No dosage adjustment is required for mild to moderate cases, but data is lacking for severe cases
Pregnant women: Animal experiments have shown teratogenicity, and contraception is necessary during and after medication use
Lactation: Breastfeeding is prohibited during treatment and for 1 week after drug withdrawal
5. Drug interactions
CYP3A/P-gp inhibitors: Strong inhibitors should be avoided in combination, and if necessary, the dosage should be reduced to 200mg once daily
CYP3A inducers: Strong inducers should be avoided in combination. If combination is necessary, increase the dosage to 800mg once daily
VI. Clinical efficacy data
NSCLC: For previously treated patients, ORR is 63% (CR 6%), with a median DOR of 38.8 months; for previously untreated patients, ORR is 78% (CR 7%), with a median DOR of 13.4 months
Thyroid cancer: ORR 89%, median DOR not reached, 100% of patients with response duration ≥6 months
Pralsetinibinformation